Ep. 20 - Melissa Callahan
Oct 12, 2020
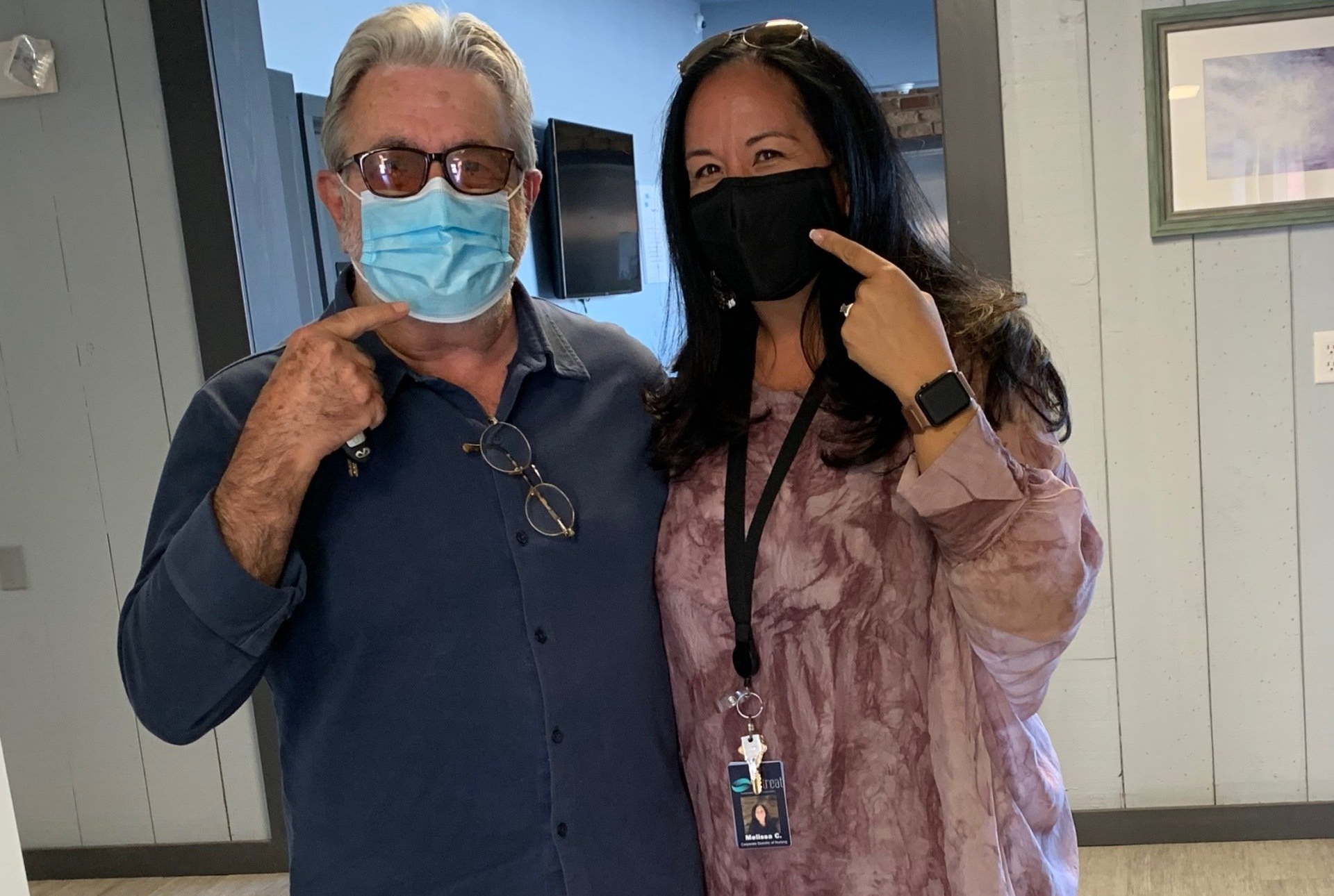
Retreat Behavioral Health’s Director of Nursing, Melissa Callahan [AGPCNP-BC, APRN] to be Promoted to Chief Nursing Officer (CNO)
(June 29, 2020) — With over 2 million confirmed cases and 125,000 confirmed deaths, COVID-19 has radically altered our nation’s landscape, but most especially, our healthcare system. Hospitals, nursing homes, emergency care, and even treatment centers have had to rapidly adjust their services. At Retreat, headlining our innovation and formulating our day-to-day procedures in response to COVID-19 has been Melissa Callahan. With her years of professional insight, her ability to remain at the forefront of all current medical and scientific advancements and her hands-on approach, Callahan has placed Retreat ahead of the game.
“Melissa’s leadership during regular times is inspiring, her leadership through the toughest of times has been nothing less than exemplary,” shares Retreat’s CEO and President, Peter Schorr, in a statement. “We have been able to ride out this incredibly difficult season with grace and ease due to the intuition and the informed nature of Melissa’s decision-making. We are in the position that we are in because of her guidance.”
With numbers for both mental health and substance abuse on the rise, the need for quality and affordable treatment is ever-more important. Retreat has continued to remain open throughout the COVID-19 pandemic, receiving patients from across the United States all while maintaining a safe and healthy environment. With incredibly rigorous everyday procedures and an executive team at the forefront of patient care in response to COVID-19, Retreat has created a strong system to combat the pandemic, with Callahan leading the charge.
A graduate of the University of Pennsylvania, holding two Masters degrees in Nursing, Melissa has practiced in Adult and Geriatric primary care with a specialty in Addictions and Behavioral Health as a nurse practitioner for over 19 years. She joined Retreat in 2014 and under her direction, Retreat has become a trailblazer in their use of Medication-Assisted Treatment (MAT) and management of compromised patients with multiple co-morbidities, which has enabled countless patients to continue to fight their addictions and remain on the path to sobriety.
“Prioritizing the relationship between clinical care and MAT services is essential to providing quality care,” shares COO, Ken Kosza, in a statement. “This harmony and like-minded consistency in our treatment process has made us incredibly strong, and we feel that Melissa is the perfect fit for ensuring our continued commitment to patient-centered care. Our team at Retreat remains committed to innovative and evidence-based practices by embracing the need for the expansion of MAT services coupled with quality and comprehensive counseling.”
In her new role as Chief Nursing Officer (CNO), Callahan will represent the nurses in the boardroom, supervise all nursing staff, maintain the highest patient safety, manage budgeting, conduct staff recruitment, and continue to expand upon personal career development.
“Addiction medicine is my calling: Although it’s not the most common specialty for many providers today, it certainly is one of the most important, helping to turn so many lives around,” shares Melissa Callahan, in a statement. “Our executive leadership has provided me with the freedom to behave as innovatively as possible. That independence has given me the free reign to structure our response and make rapid-fire decisions based on the most relevant medical and scientific information currently available. I am honored to work alongside our incredible team and look forward to all the growth yet to come as we continue to raise the bar for what high-quality, innovative treatment can look like.”
# # #
EDITOR’S NOTES
For more information, please call 855.802.6600, or visit our website at https://www.retreatbehavioralhealth.com/, or connect with Retreat Behavioral Health on Facebook, Twitter, LinkedIn or Instagram.
Retreat Behavioral Health is a healthcare provider based in Palm Beach County, FL, operating large residential and outpatient treatment sites throughout Florida, Pennsylvania, and Connecticut. Retreat specializes in substance abuse and mental health care services.
For media inquiries or more information, please contact:
Marissa Hayes – Corporate Director of Communications
Email:
marissah@retreatmail.com
Ep. 20 - Melissa Callahan Interview Transcript
The Behavioral Corner: 0:08
Hi, and welcome. I'm Steve Martorano. And this is the Behavioral Corner; you're invited to hang with us, as we've discussed the ways we live today, the choices we make, the things we do, and how they affect our health and wellbeing. So you're on the corner, the Behavioral Corner, please hang around a while.
Steve Martorano: 0:27
Hey, everybody, hope you got a sweater on as we hang on the Behavioral Corner. I'm Steve Martorano. We're gonna see who crosses our path here. What we're doing, I hope you're aware by now is that we talk about behavioral health, big topic, a big topic, a topic that put simply, I guess, deals with the way we behave, and how that impacts our emotional, psychological and physical health. It's a big field. It's covered by lots of people, not least of which our underwriters and partners in the program Retreat, Behavioral Health. So we reach out again to them because they have the best people with the best information. None more show than our guest. Melissa Callahan, Melissa is the chief nursing officer for retreat behavioral health in that capacity. She oversees a lot of stuff regarding their facilities in the Lancaster County area, Florida, as well as Connecticut. She's a longtime contributor to the program. And she's absolutely my go-to person. When I got a question about COVID-19. I don't, yeah, I read a lot of stuff and you know, ignore a lot of stuff. But when I want info that I can absolutely rely upon, I always call upon Melissa, thanks so much for joining us again, good to see you.
Melissa Callahan: 1:46
Thank you for having me. I always love to come and chat.
Steve Martorano: 1:49
Well, I know how busy you are. So let's really dive right right into this. Melissa was among literally among the first healthcare professionals, who I was aware of who was saying, hey, this thing is coming. And it's serious. I mean, a long time before you were hearing about it, in the newspapers and on television. So she got my attention then because she was right. And I'm sure she'll be correct again today. Up. So we're, you know, the winter we're talking about the winter of our problems coming forward. Now. We're trying to get our heads around, well, how it's not going away? What's it going to be like? And how do we prepare for it in the coming fall and winter months? So Melissa is here to help us with that. So let's begin at the beginning. Where are we with regard to the first wave? Are we at the end of the first wave the middle of the first wave, beginning of the second wave? Where are we?
Melissa Callahan: 2:40
By no means believe that I am an infectious disease guru or a scientist who's been working on this continuously. I try to keep myself educated and in front of everything, medical and scientific-based when it comes to the pandemic that we're in right now. I hope that we are trending down. I don't know how many waves are a part of COVID-19. But I do believe from all of the literature reviews that I've done and speaking to colleagues on all the coasts and even internationally, that there is a weakening of the virus. I don't look at the numbers and statistics. I don't focus on those I see them but I don't focus on them to make the judgment. I know that as people started going back into workplaces and school environments, numbers went up. But I also through my research, realize that the hospitalizations did not correlate like it did when it first arrived. Or we first started speaking of COVID-19 in the United States.
Steve Martorano: 3:43
So if I understand you while we see a greater incidence of community spread of this thing, because of contact, we're not seeing a corresponding spike in hospitals,
Melissa Callahan: 3:54
Not from what I can see in the research, it may be out there and we may see it coming down the line because it takes a long time to really aggregate this information. Some information gets pushed out real quick because you want to get answers and try to come up with resolutions to keep people safe. Because of the safety of people is the most important thing. And I think people are doing the best they can to get it out there from everything that I'm looking at. We see the numbers, we know that they're up there, but the hospitalizations, the capacities filled in the hospital settings are not near what they were, I believe in March, April, May.
Steve Martorano: 4:29
Well, you know, and we've lost sight of the fact that at the beginning of this thing, at the height of it the worst moments, it was maintaining the integrity of the health care system, particularly the hospitals. That was the goal. The goal was we weren't gonna be able to stop the spread. But if the health care system had collapsed, correct, then a lot more people would be dead correct. So that's what social distancing and for God's sake, that's what is about. You know, wear a mask and wash your hands for crying out loud. Anyway, we're here we saw a wave doesn't seem to be rising. But who knows? The idea is to continue doing what we're doing. From a healthcare perspective, when you say, you know, you can't read all these numbers and make a lot of sense out of them as a healthcare professional, you then look at what's happening right in front of you. Yes, right in front, what's going on around me and my community that guides you and where we're at? Absolutely. So we don't know about a second wave. Certainly. It's flu season. And I think that's what's got a lot of people have freaked out. So you advise people, of course, get a flu shot?
Melissa Callahan: 5:33
Absolutely. Absolutely. There are many forms of the flu shot now. So, people who were allergic to the egg in the past and couldn't receive it, there's now cell-based so you can have it if you have an allergy to eggs, some people who had allergies to different antibiotics were steered away from getting the flu vaccine, but most people in the population really would benefit from having the protection of the flu vaccine.
Steve Martorano: 5:57
What about and I asked my doctor about this for seniors, and pneumonia shots?
Melissa Callahan: 6:04
Yes. So the recommendation is over 65? Absolutely. You should have your flu shot every year, and you should have your Pneumovax, which I believe is every 10 years at this point. And anybody under 65, who's actually had pneumonia should have the pneumonia vaccine.
Steve Martorano: 6:17
Shouldn't people also make sure that they're on the same page with their primary care physician in what kind of pneumonia drug they took? Because they told me they had to check on when I got those 10 years? She said you're okay not to worry about it. So it's important to know that, but there's going to be a flu season is not going away. We're gonna already here we're gonna have a flu season, how do people distinguish between I've got the flu. And "oh, is this something worse?"
Melissa Callahan: 6:46
I don't know that we are going to be able to distinguish as laypeople or even providers without doing some diagnostic tests, distinguishing one from the other. There are very similar symptoms for both fever, coughing, sore throat, fatigue, there are so many overlying features. If you are sick, the most important thing is to stay at home. Don't go into your work environments. Don't go into schools, wherever it is, and notify your health care provider, take the guidance from them. If they feel as though you need to be tested and which test you should have. We may get lucky this flu season because people are encouraged strongly to wear masks wash their hands and social distance. Maybe we can actually decrease the number of influenzas that we experience every year in the United States. Because these are good health practices. The common cold coronavirus, people usually get a couple every year they're used to it, they move on, we're much more aware, maybe we can cut them out completely minimize them as much as possible while decreasing the spread of flu and COVID-19.
Steve Martorano: 7:54
You know, anybody that's watched anything over the past 10, 20 years, in terms of other cultures and how they behave? ordinarily, for instance, in Asia, wearing a face mask is nothing unusual. They've been doing it for years and years. Are we now in a moment where we're going to pretty much have to modify our behavior and just wear masks in dangerous periods of time, like any flu season?
Melissa Callahan: 8:21
I think it's smart. It's not an unsafe hard choice to make. And it does really improve your protection. There are many people when they just get on a plane or go into these real tight environments like concerts and sporting events, which I know so many of us to miss because they have not been in our everyday life. But it is thought that we know there are airborne germs, we know they spread very quickly. It's microscopic, you don't even know it's there. Potentially they live on surfaces. And I think we are going to see masks for a little while in the future. I don't know how long it really will depend on what social media puts out there on effectiveness. And when things are moving along. If we believe that COVID-19 is no longer a threat or a threat at the level that it has been in 2020 you're going to see it dissipate. And some people right now they really don't believe in it. They feel uncomfortable with it. And unfortunately, there's a lot of fear around COVID-19. But I think what's most important to tell people is it doesn't hurt to put a face covering on just like it doesn't hurt to wear shoes and it doesn't hurt to wear a hat in the winter. If we can try to make it as simple as that. Yeah, I think can make it more compliance but it's working. It's definitely working
Steve Martorano: 9:39
It is working and we look at the worst examples and how they overcame it. I mean, New York City, New York City alone is a remarkable people want to understand New Yorkers. New Yorkers look crazy and act crazy and they live in a crazy environment. But New Yorkers sort of know what it takes to survive in a packed metropolitan area. So when they were told to stay in and wear masks, they did!
Melissa Callahan: 10:00
It's actually unbelievable. You know, some people really focused on some of the negative parts of being forced or told what to do. And I focus completely on the positive parts that just slow down a little bit and take a breath and kind of reevaluate what you're doing every day and how you're doing it. And there are so many positive things that have come out of that I think families reconnected, I think that workplace environment and priorities reset themselves. And there's nothing wrong with that.
Steve Martorano: 10:31
Nothing at all. Nothing at all. And when was it ever a good idea to sneeze in someone's face? I mean, it's just ridiculous. Anyway, let's try to make this a real-world experience. So it's October here. Now as we speak, and flu season upon us, a virus loose in the land, like, you know, someone wakes up, headache, their achy, throat hurts a little bit, maybe they have a fever. They call their doctor, at what point does the physician say you need to get into a hospital? Is it a breathing situation? Is it the height of the fever, what would...
Melissa Callahan: 11:06
So it depends on the person, it depends on what kind of medical state they're in, to begin with if it's a young, healthy person, I think most providers are going to tell you to push fluids, stay home, rest, make sure your diet is pretty high in vitamins, vitamin C, all-natural immune boosting behaviors. And if the fever goes over 100 is 100.5 is what they look at for COVID. But it has to be a sustained fever, not just a one time fever if you get up and take your Tylenol or Motrin, and kind of rest the day away. If you're feeling better, within 12 hours, the next day, the probability is it's a short-lived virus, it's not a virus like the flu or COVID. Because both of those seem to progress pretty quickly. So the symptoms generally are not just resolved by a Tylenol or Motrin or a day of rest and trying to just recuperate your immune system. providers, I'm sure to have algorithms for their nurses and their triage, and they're getting the phone calls to make a decision in certain areas. If you're starting to have a lot of positive cases, you're going to be a little more aggressive with testing. Most times, they don't want to bring you into the office if they think you have influenza or obviously COVID-19. But depending on the area, you're in the Department of Health has a pretty good algorithm of who should be sent where testing is best, and what parameters to use in order to test people.
Steve Martorano: 12:33
Age is a big factor. If you have any of these symptoms, and you're over 65 that's going to involve a little more proactivity, I would guess Yes. And breathing is a big deal. This thing is a lung killer. trouble breathing, I guess would be a red flag. But we don't want what we don't want is to have people show in the dark and fearful and confused that they begin flooding the emergency rooms of the country because that's a problem we need to avoid.
Melissa Callahan: 13:01
I agree. I think that people are a little bit passed that I think more people I find are in denial that it's not really here anymore. They don't really have that. And they're the people I'm fearful of that are just going out and about. And when they go into somewhere and they're asked the questions, they're so quick to say no, no, no, and not really listen to what the questions are. Because the questions aren't always just Are you having these symptoms, they're oftentimes now including, are you in close contact or living with someone who has any of these symptoms, because the young healthier person could live with mom and dad, mom and dad could have the symptoms and then be positive, and then you're asymptomatic, but you're carrying it. And then as you're running out and about feeling like I feel fine, I'm good. Exposing other people.
Steve Martorano: 13:49
We're talking to Melissa Callahan, Chief of a nursing officer of retreat, behavioral health. She is with us very often here on the behavioral corner, helping us get our heads around what we need to do because now we see what we're up against. We have best practices, we know what they are. They're not hard. And the winter's coming. So we're going to be locked up together. And it's the worst conditions for this virus.
Retreat Behavioral Health: 14:12
At Retreat Behavioral Health, we believe in the power of connection and quality care. We offer comprehensive holistic and compassionate treatment from industry-leading experts. Call 855-802-6600 and begin your journey today.
Steve Martorano: 14:31
You mentioned testing though, you said they'll determine which type of test tell us what you mean about types of tests.
Melissa Callahan: 14:38
So testing has been really difficult throughout this process. And it's been difficult because we definitely don't have enough information to create a great perfect test. There have been many tests that have been produced, some have made it to market have been pulled back. There are tests that can be done that's by your saliva. There's a test that can be done in your nose. Sometimes it's the lower end of your nose, sometimes it goes up and it gets your nose and the back of your throat, which is your pharynx. There are also blood tests that can be done. Throughout my research, I have found a lot of inconsistencies because there are so many variables that can make these tests effective and efficient or not. Some of it is the way the test is taken. Like if it's the swab test, if you didn't swab well enough, you can come up with a negative when someone's really positive. And so there are variables that you have to be cautious of. And unfortunately, I cannot say that there has been one test that has been the gold standard, and has been tried and true and has given us the best outcomes. But I am confident in the scientists and doctors who are working aggressively to come up with something that all the things put together, we're going to have a pretty good idea of testing. But I will tell you, there have been people who've been tested multiple times. And sometimes they got a positive than the next one with a negative and it's hard to know, it really is hard to know.
Steve Martorano: 16:02
Yeah. So so difficult. The turnaround time is, you know, self evidently true that if you can't get the result. First off, if you can't trust the result, that's a problem. But even if you could, the turnaround time is critical. Because if it's not pretty immediate, right? And you're going to risk being exposed again, it's very difficult. You know, it seems to me, and I've thought about this and thought about this. It's nothing that you could do effectively on the fly. This is something that we should have been. It's not like people weren't warning about a pandemic, they would. Hollywood had made 20 movies about this stuff and everybody, you know what? Oh, yeah, really, we knew was coming. So we should have been way, way, way ahead of the curve on effective testing. Well, we're gonna get good at it. Now, I guarantee you that let's talk about, again, some of the practical things about getting ready for the winter. You know, everybody should have a home first aid kit. I mean, and I, if you're like me, it involves some ointment that you bought over the counter. Lots of band-aids, yeah. When when I was a kid, we always had to stock up MercuroChrome. Yeah, whatever that was...
Melissa Callahan: 17:08
I have not seen that.
Steve Martorano: 17:11
...and maybe some cough medicine, what do we need in a really effective home first aid kit.
Melissa Callahan: 17:18
We definitely need to add masks. Masks are definitely something that you just can't go wrong, having it with you and having it nearby, we've created these little packages within my house, every car has one. All my kid's baseball bags have one because you never know when you're somewhere and you can't get in without having the mask on. Or you might be in a tight quarter and you just want to have a little bit of space is extra protection. So I think having masks very important. Hand sanitizers are also very important and very easy to have right on hand. We know that you know, over at least 65% alcohol is what the recommendation is. So hand sanitizer, mask. I think they're good additions to have in this flu season and COVID-19 of 2020.
Steve Martorano: 18:04
Yeah, I can't tell you how many times I've seen people do it stop dead in their tracks and turn around, go back to the car. And I know they're doing what I do as well. You forget your mask. Somebody said to me, "Yeah, Batman has been putting up with this for a year." Jump in the car and go, "Oh, I forgot my mask." You know, have them in the car, we have a glove compartment filled with. Obviously, everyone likes to have a state of the art mask. But I mean, a lot of things work, what doesn't work?
Melissa Callahan: 18:29
So there's a lot of talks that a bandana or a cloth is not nearly as effective. And we know definitely the thread count is not meant to prevent certain microbes of germs, obviously. But any covering on your face is a protection versus nothing. A regular old medical mask a medical, there is two or three-ply. They're excellent. They're perfect. You can get them on Amazon and everywhere. I asked that people really reserve N95 and higher-level protective equipment for health care providers in the hospital settings where there's definitely active disease and close quarters that you can't really get away from. So I don't think the average person should have a high level. But any face-covering any face covering is effective, more effective than nothing. And like you said earlier, I think they probably taught people how to cover their mouths with coughing and sneezing since the time that they were all born. But the average person is not conscious of that act. But nowadays, one sneeze everybody looks and automatically has a look of Do you have COVID? It's actually forced people to be mindful to actually be conscious, and not just sneeze out in the open because MIT has done plenty of studies and we know these droplets are going all over the place. So, another silver lining.
Steve Martorano: 19:51
Yeah, no, really. I am the madman of the house. I mean, somebody sneezes in the other room. I'm yelling, sneeze outside. What
Melissa Callahan: 20:01
It's true.
Steve Martorano: 20:02
He's outside, don't sneeze in here. You know, the other thing is are always nice. Well, yeah, he always leaves. But if you're, if you're contagious, it's terrible. So it's amazing how you were back to some of the most fundamental things.
Melissa Callahan: 20:15
Let's talk about wash your hands. So when I went into nursing school, I did my bachelor's at Penn State, one of my very first clinical sessions, you had to wash your hands in front of your clinical instructor and pass that assessment skill prior to going to any of the next levels. And I thought it was so ridiculous. But then I also remember being nervous, going through the steps, and counting in my head, how I was washing every surface, I was getting my nails in between my fingers. And, and I would laugh at it. And to this day, we still test every nurse doing that. But if you look at the average person, they don't wash their hands correctly.
Steve Martorano: 20:55
Run their hands under some water.
Melissa Callahan: 20:56
Yes, anything that's washed.
Steve Martorano: 20:58
Yeah, our studio is in one of the facilities of Retreat. And this is well before COVID, there's a large assembly room, around the corner here. And often, you know, you do some training in there. And I walked by the open door coming to the studio, and I heard the topic, which was hand washing. And as I got to the studio, I did exactly what you did, given that retreat handles people with, you know, difficult emotional and mental issues, but a lot of substance abusers who are desperate straits, and I'm thinking they're telling him to wash their hands. How was that all about? Well, that's what it's about. I mean, wash your hands, just like mom told you to wash your hands. It's ridiculous. Well, we're getting better at that. That's, that's for sure. Let's talk about kids. They may be going back to school, someone a hybrid situation. Are you confident that we're okay to have them back at least in some fashion, as we head into the fall?
Melissa Callahan: 22:01
I am. And that comes as being a mother as well as being in health care. I think that we need to focus on not only the physical and the pathophysiology of COVID-19. But the mental health of everybody in society. My kids are fortunate that they've been able to play sports or outdoor sports since June. And I think that that has done amazing in terms of their mental health and their physical activity. They've gone into the school year purely virtual, they are so excited to have the hybrid opportunity. Because we need to have human stimulation, we need to move. What virtual has created not only has it isolated people, but they're immobile. My children are sitting in front of a screen for seven hours straight, I had to buy them all blue light glasses because of the fatigue in their eyes. And so I think on a mental focus and a physical focus with the parameters that have been in place because I think the school districts have been amazing in creating the safest possible environments, they can that it is time to start integrating as much as we can really see where the numbers are, be really conscious have really good plans. If numbers occur if positive cases begin, not just jump right back to isolation. Okay, what are we going to do? Is it a three-day cycle, you do cleaning like I said, the school districts have spent so much time taking into consideration every type of family, every type of child and creating the safest possible environment. And there's going to be a time that we have to do this. We have to go from complete isolation and start bringing people into populated settings. And I think that for the mental health and for the physical movements it's time.
Steve Martorano: 23:59
Yeah, I'm glad you brought that up. October is National Mental Health Month. And we're focusing on that here on the Behavioral Corner as well. It's a large component of not only, you know, your everyday well being that you'd be balanced mentally, but there is a mental health crisis correct going on now, and we need not forget about that. Parents are particularly stressed. What advice do you have as a healthcare professional on parents who like may get it wit's end about all of this?
Melissa Callahan: 24:32
Be really mindful of self-medicating, and self-medicating can be from food to alcohol to actual medication. People choose all those different routes. Be mindful that you're not trying to handle and deal with things in a poor self-care manner. Make sure that you yourself are moving drinking fluids, eating well, creating schedules so that you can be a professional if you're professional or be a homemaker. And having your children there and having, you know everything in a virtual presence, because I think parents spend most of their time trying to tell their kids to get off of electronics or get off of computers. And we have thrust them into more than 60% of their day, being focused on that. Some of my kids have been like, maybe we can just get a book because they're doing everything virtually, they're actually printing things out. So they can write and use a paper and just kind of mix it up a little bit. So I think that parents continue to be patient, you're automatically patient. Once you become a parent, even though you believe you don't have patients you do because you have a child. So it's automatically becoming part of your every day, be really mindful of your self-care, be really mindful of self-medicating. And, you know, I say simple as food, because people don't realize that they might be stressed eating, they may be eating unhealthy choices, because it's quicker, it's easier, because of the changes in their life. But the kids have been unbelievably resilient. So they're teaching us resilience because we at one time had that. And if we can find our way back to that, we'll get to the other side of this and realize, I think some of the silver linings, like I said, Yeah, slowing down a little bit. reevaluating priorities.
Steve Martorano: 26:21
Kids really roll with the punches. It's amazing to watch the and the younger they are they seem to be more understanding about that. Let's take a moment here to talk about people who are inactive recovery, but are stressed beyond belief in terms of what they should be paying particular attention to during the fall and winter, and COVID, what advice would you give them?
Melissa Callahan: 26:43
Make sure they stay connected, I do see a lot of people are starting to struggle with everything just being zoom. And they found really creative ways to go to parks, and it'd be an outside setting and trying to have meetings and fellowships in some setting. You cannot isolate. And you cannot just believe you can do it on your own. If you were in an active program, you have to continue that program. If you have to alter what that looks like, because of the changes that have occurred around you, you have to stay proactive for your recovery. If you get complacent, then, of course, bad things can happen and mistakes and errors in the wrong places wrong time. And, you know, compromises can happen. And that's for someone in recovery as well, someone, not that's just if anyone gets complacent, it really can create negative behaviors.
Steve Martorano: 27:33
Well, as I suspected, that Melissa Callahan comes armed with just her experience, expertise, and common sense on things that we have to do to make sure that COVID which is already devastated the world in this country doesn't have its way with us again, as we enter the flu season. And I thank you for your time your very busy lady. I detect the kind of hopefulness in your conversation here today. And I know you're not a Pollyanna kind of person. You're the one who sounded the alarm early, like come on. Let's get ready for this. See what happens now. So you're not painting a rosy picture here. Except for the fact you think if we do things the right way, we don't have to be terrified. Is that what you're saying?
Melissa Callahan: 28:16
Yes, yes. It's unfortunate that fear makes us just not think clearly sometimes.
Steve Martorano: 28:23
It's stupid. There's no doubt
Melissa Callahan: 28:24
It definitely it clouds what your thought process is and cause and effect and fears, terrible way to live. And I think it's important to understand the enormity of what has happened and what we've lived in. But know that we have to continue to put one foot in front of the other and move on and it's going to create some innovation, it's going to create change to our every day. And that's not a bad thing.
Steve Martorano: 28:51
No, it's not. We once had an example of how important managing fear is when a great president once said that the only thing we have to fear is fear itself. Well, that's not technically true here. Now we do have something actually to fear. But it shouldn't, as Melissa just said, immobilize us and make us do foolish things. Melissa Callahan, it's so great to see you again. You're a deli ht and you lift my spirit. ou really do and we hope we can call upon you many more times here on the corner.
Melissa Callahan: 29:23
Of course.
The Behavioral Corner: 29:30
That's it for now. And make us a habit hanging out at the Behavioral Corner. And when we're not hanging, follow us on Facebook, Instagram, and Twitter On the Behavioral Corn
Subscribe. Listen. Share. Follow.
Recent Episodes