Modern Psychiatry. It’s a long way from Dr. Freud.
Oct 24, 2021
Dr. Jonathan Beatty, Wave Treatment Centers of Philadelphia, is treating addiction in exciting ways. Exploring underutilized therapies for addiction, this time on the “Corner.”
The Behavioral Corner Podcast is made possible by Retreat Behavioral Health. Learn more:
https://www.retreatbehavioralhealth.com.
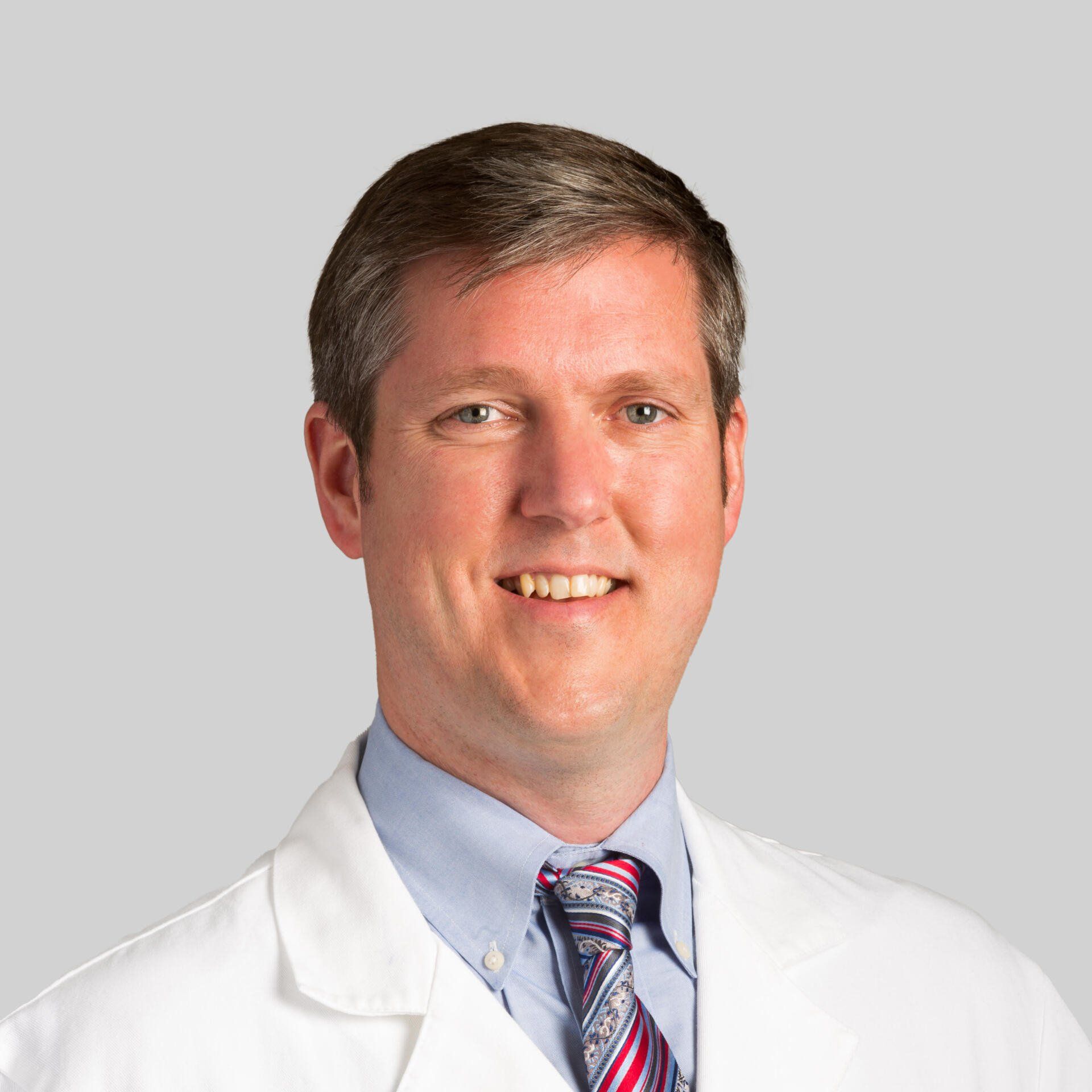
Dr. Jonathan Beatty, MD
American Board of Psychiatry & Neurology
American Board of Pain Medicine
American Board of Addiction Medicine
Dr. Jonathan Beatty, MD
Dr. Beatty is the founder of Wave Treatment Centers. Dr. Beatty is triple board certified in the field of Psychiatry and Neurology, Pain Medicine and Addiction Medicine. After his internship at Louisiana State University he completed his residency in psychiatry at Hahnemann and Drexel University where he took additional training in neurology and pain medicine. Additionally, he spent two years working at the Institute of Addiction Medicine where he apprenticed under Joseph Volpicelli, M.D., Ph.D. Dr. Volpicelli is a Master Clinician and true pioneer in the field and an unparalleled teacher.
Dr. Beatty began his career as a faculty attending physician at the prestigious Thomas Jefferson University where he served in several roles across hospital and outpatient as well as bedside and classroom education. He helped expand their pain medicine program before he was recruited by a leading national private addiction treatment center conglomerate to be the psychiatrist in Chief for their Northeast division. In that role he helped implement mental healthcare best practices to an existing facility as well as create a build the medical infrastructure and programming for a brand new inpatient facility they were starting. After deciding to go into private practice Dr. Beatty opened his first office in center city Philadelphia in 2014 where he still holds part-time hours. Dr. Beatty always wanted to return to his hometown of Chestnut Hill and opened Wave Treatment Centers in 2019 when a beautiful office space became available on the corner of Germantown Avenue and Willow Grove Avenue. The goal of
Wave Treatment Centers is to implement the highest quality of care and implement specialized medications and technologies of this rapidly evolving field. Dr. Beatty is continuously furthering his training and education in order to deliver the best care and safest approaches available in the outpatient setting. Dr. Beatty is also on staff and has admitting privileges at Chestnut Hill Hospital should a higher level of care become necessary.

Wave Treatment Centers
Wave Treatment Centers is a premier provider of outpatient addiction and mental health in Philadelphia, PA. Led by physician Jonathan A. Beatty, M.D., a Fellow of the American Psychiatric Association (FAPA), Wave specializes in Transcranial Magnetic Stimulation (TMS), esketamine/ketamine, medical detoxifications, and long-acting injectable maintenance treatments. Our staff are not only highly educated and credentialed, but they are also compassionate, caring, and supportive. They devote their time and expertise to helping those looking to reclaim control in their lives once and for all.
Contact
215.242.0420
Wave Treatment Centers
6 E. Willow Grove Ave.
Philadelphia, PA. 19118
Wave Treatment Centers
407 S. 10th St.
Philadelphia, PA. 19147
Ep. 74 - Dr. Jonathan Beatty, MD
The Behavioral Corner
Hi, and welcome. I'm Steve Martorano. And this is the Behavioral Corner; you're invited to hang with us, as we've discussed the ways we live today, the choices we make, the things we do, and how they affect our health and wellbeing. So you're on the corner, the Behavioral Corner, please hang around a while
Steve Martorano
Hey, everybody, welcome again to the Behavioral Corner. Here we are hanging I'm Steve Martorano, on the Corner all the time. As a matter of fact, I spend more time on the corner than the newspaper box. And I'm lucky because I always run into great people who have I think, interesting things to tell us and information to share. So we're no different today here on the Corner. It's all brought to us by our underwriting partners to Retreat Behavioral Health. Listen, I got a fascinating one for you today. I am really looking forward to talking to our guest, Dr. Jonathan Beatty. Briefly, he is a psychiatrist and I will give you his full resume in a second. But psychiatry is so fascinating. At least it is to me I have never been in need of psychiatric help. <<knock knock>> Knock wood. I get my information the way a lot of us do through the media. I think I know what psychiatry is. Certainly, Woody Allen has spent 100 years telling us what it means to him. And we all have seen every actor in the world play, Freud. So we know about the couch, we know about the chair, we know all that stuff. But really, what we want to do today is take what not a deep dive because we don't have all day, but certainly, get our feet wet on trying to get our heads around modern psychiatry right now in general, and something called neuropsychology, which is we'll get a little more specific about straight ahead. I want to thank Dr. Jonathan Beatty for joining us. Dr. Beatty is a Board Certified psychiatrist and neurologist. He is board-certified pain medicine, as well as addiction medicine, and we welcome him to the corner. Doc, thanks for joining us.
Dr. Jonathan Beatty
Thank you for having me, if I may, just a brief clarification. I'm board-certified by the American Board of Psychiatry and Neurology in psychiatry. So the idea of neuropsychiatry is valid, but I wouldn't, I'm not separately boarded in neurology, just...
Steve Martorano
Terrific. I can't think of anybody, given the current state of affairs who would be busier than a psychiatrist. So thank you, thank you for your time. Let's begin there with you know, the term I'm least familiar with. And that is neuropsychiatry. What is it? And what do you do?
Dr. Jonathan Beatty
So, I guess, to backup neuroscience, which is one of the basic sciences that we learn about in, you know, to some extent in college and often in graduate school programs or doctoral programs, as well as part of the basic science course in medical school. So neuroscience is kind of the study of the brain from various anatomical perspectives. So the physical tangible, what is in the brain, you know, I was telling you earlier, this is, you know, a plastic model of a brain and, you know, if you dissect it, what's inside it.
Steve Martorano
My brain feels like that, just now we twisted this
Dr. Jonathan Beatty
The little part, right.
Steve Martorano
Yeah.
Dr. Jonathan Beatty
Neuroscience from an electrical standpoint is often more thought in terms of neurology, at least historically. And then from a sort of what often is commonly referred to as a chemical standpoint, which is often in the realm of psychiatry. So the reality is the same brain, right. And the brain communicates with itself and with other parts of the body, through both electrical signals, and hormones. So the neuro train and neurotransmitters, so the neurotransmitters, the ones you hear about a lot in the media, probably dopamine, norepinephrine, serotonin, people have this idea in their head of this, you know, chemical imbalance. And that's, that has become people imagine that, and it's a really good image that makes sense, and that you can explain to people, it's not entirely accurate, but at least it sort of explains a little bit about what's happening inside your brain. But again, that's from a neurotransmitter perspective. There's also an electrical aspect of the brain. So each communication is because of a low voltage system that basically either activates or inactivates certain channels or certain, you know, ion influxes of positive and negative charges that then open and allows the neurotransmitters to go through from point A to point B. So all of that together is kind of neurology, and then the behavioral aspects or the outcomes of those interactions, you know, is kind of psychiatry. And so I suppose the interface of those two would be neuropsychiatry.
Steve Martorano
Yeah, I was reading up on it a little bit last night. And while the two disciplines or fields have been around for a very, very long time, they sort of separated in a sense, a while back, and now they're slowly coming back together, and that's where I guess we get the idea of neuropsychiatry. How closely are they getting now?
Dr. Jonathan Beatty
Right. So that's a good question. And just to, you know, explain the board of the American Board that I alluded to earlier of Psychiatry and Neurology, it's a combined board. So there's always been a recognition that these two things are together. But there's been sort of a little bit of a separation between them, that probably stems back from Sigmund Freud, who you alluded to earlier, who, you know, kind of started the field of psychiatry in many ways, in terms of the behavioral aspects of the brain, he was a neurologist, and, you know, he was more focused on the intangible qualities of the brain and how they, you know, at that time, they didn't understand anything about the connections in the brain, you know, it was really just neuroanatomy, there was no real understanding of the physiology of the brain. So he looked at behavioral aspects and sort of postulated what could be driving those. So these unconscious wishes and things like that. It has continued, but it has sort of continued in parallel with neurological sciences in the sense that not necessarily disputed or refuted, but it wasn't necessarily congruent with everything that was starting to become discovered. And interestingly enough, now there are some connections that may explain some of those behaviors that he was describing now through more of a physiological lens. And so that I think is how psychiatry is moving forward in terms of not just, you know, talking about what's going on, although, you know, that is a very important aspect to understand. It's one way that we can access the brain, in a sense and understand at least through the language, what the experiences are, and then through certain neuroimaging technologies, like functional MRIs, and PET scans, which are two types of ways that we can look at the brain function. In other words, while you're talking about your childhood, which part of your brain is active, and which party raises inactive, when you're thinking about a drink, for example, in an alcoholic, which part of your brain goes into hyper mode and gets really excited just looking at a picture or watching a commercial or whatever, with an alcohol bottle? That gives us a sense of what's going on in the brain in that part? And then how can we maybe modulate that piece of the brain or that overall interaction between the different parts of the brain in a way maybe through talk therapy, maybe through pharmacology, such as certain medications, or maybe through brain stimulation techniques, and these things, I would say, are moving the field forward at a very interesting pace, and are allowing us to deploy new understandings of the brain and the connections between the brain to develop new techniques to treat things in a more kind of modern way, I suppose.
Steve Martorano
Yeah, a scientific way. I mean, there have been techniques that have been successful in the past. And now there are new and even more exciting techniques that are being employed. Let me just say this about a classical analysis --- psychoanalysis. seems obvious to me that if Freud had done what he did 100 or so years ago, today, it would never have risen up the way it did today would have just been No, no, you're groping around in the dark. Here are some of the places to be looking to explain this behavior, not where you're looking. Right?
Dr. Jonathan Beatty
Right. I think that's a very good way to conceptualize.
Steve Martorano
And I will and then we'll go on to some of the things you treat with neuropsychiatry. I think it was because of that -- tell me if you agree -- that we get this notion that certain behaviors even addiction are somehow rooted in character or free will or choice made poorly. And it's taken a very long time for science to turn around and say, yeah, listen, it's not about a fraud their character their behavior is being affected by something going wrong in their brain.
Dr. Jonathan Beatty
Absolutely. That's a great example actually because if you look at addiction obviously has been around probably since the invention of alcohol and even before that with opium and you know, poppy plants when they discovered what those can do, and to some extent, even with the caffeine, you know, with the coffee bean so you know, these are things that when you look back at when people started paying attention to this and it became a societal problem. So that was recognized before there was a science to explain it. And so it was what else do we call it? Well, just don't drink anymore. And you know, like, you don't have that you must be lacking in willpower somehow that you have a moral deficiency, you're a bad person and even the language that still permeates the culture which is clean and sober, right? So what is the opposite of clean and sober, dirty and drunk I guess so? You know, there's this implicit bias that you're only clean you know, you just got out of the shower, you're clean if you're sober, but think about what that means for the people that are struggling with addiction, they're being told that they're not clean. You know, I mean, that's, that's awful. That's just demoralizing. If anything, that's the character flaw, not the person with the struggle. It's the, it's the people that are observing it and calling it something, it's a judgment really
Steve Martorano
disingenuous. And it's almost easily understood in the sense of, it's kind of a defense mechanism by the rest of us, that's not going to happen to me, because I'm not that kind of person. So I sort of get that. But anyway, it has set us way back. And now we're starting to catch up
Dr. Jonathan Beatty
Now that science can show us that there's this pleasure reward pathway in the brain that goes haywire when a substance of sorts is introduced to the system to the brain, so to speak, that part of your brain that is designed for survival. So for food and sex, basically, the things that would promote our survival in order to pass on our genes, which, evolutionarily speaking, is essentially why we're here, not very romantic, I realized, but from a brain biology standpoint, that's what that part of the brain does. If you introduce a substance, be it alcohol, or you know, even nicotine, frankly, which is also obviously highly addicting, that does a lot to that pleasure reward pathway in the brain, and it skews it completely to favor that particular, that substance. And what we've also more recently learned is that there's an anti reward pathway, which is what gets activated as you withdrawal from those substances. So when you become physiologically dependent on say, heroin, or alcohol, or even nicotine, nicotine is a good example of coffee, people are cranky in the morning before they have their cup of coffee. That's caffeine withdrawal, that's the anti reward system, coming online and becoming activated and making you irritable, and people will go out and get a cup of coffee when it's caffeine. But when it's something a little stronger, like heroin, they'll plunder to get to another dose of that, and you know, in that it's to avoid that anti reward pathway. And that's, that's one of the really important details of the imbalance in addiction,
Steve Martorano
And why we can hopefully look to something like neuropsychiatry to help us get to the root causes of these things. And maybe, you know, maybe adjust that behavior, because it's always struck me as particularly cruel and scary fate, to have a problem, the origin of which is in your mind, your brain, I should say. If you're diagnosed with cancer, overwhelmingly, your brain focuses very specifically on what should I do to save myself. But when the problem that you're dealing with is, is a miss function of the brain? What tool do you use? Because as you mentioned an addiction, you know, you're being told there is no problem or mood disorders, you're being told. There's nothing wrong with me, everybody else's sort of crazy,
Dr. Jonathan Beatty
How do you self-advocate when the self-advocacy party is functioning? Right?
Steve Martorano
So tell us, if you might, this is a brand-appropriate moment, the sort of things you would treat as a neuropsychiatrist.
Dr. Jonathan Beatty
As I alluded to addiction as a big is a big part of what I do. That has certainly overlapped with neuropsychiatry, but I would say some of the other sorts of areas outside of addiction that are a big component are again behavior so that what is the driving force, what is the inactive or underactive or overactive part of a brain that we could potentially identify and then do something about to change either a behavior or mood symptoms, say like depression or anxiety, or maybe a memory problem like Alzheimer's, dementia, or even a movement disorder like Parkinson's or, you know, a migraine headache, even. You know, some of these things which have more clear physiology. And by clear, I mean, more well-known or well understood, and then some of the things that are a little bit less are understood, but at least we get the concept of where they take place. So one of the things that I do, for example, is TMS, transcranial magnetic stimulation. So that's a form of brain stimulation, which is very different from one of the more well-known forms of brain stimulation, which is called ECT, or electroconvulsive therapy, what people used to call shock therapy. So shock therapy in that sense, which was an electrical shock, or even many, many years ago, they don't do it anymore, there was actually insulin shock therapy where they would use insulin to lower your blood sugar, which would cause basically a seizure. So ECT, the shock therapy through an electric convulsion, and insulin shock therapy, which again is no longer used anymore, because depriving cells of glucose is a bad idea, especially in the brain. The end result was a seizure. That seizure, you know, again, electrical, the brain is an electrical organ. So the seizure activity seemed to sort of reset the brain and it was a global seizure. I mean, and in the earlier days of ECT, and again, this is different from what I do. I'm setting up a distinction here. Sure, in the older days you would see the entire body convulsing.
Steve Martorano
It's what Nurse Ratched did.
Dr. Jonathan Beatty
Yes. And unfortunately, that movie set back psychiatry quite a bit. I mean, even to this day, people asked me about that I'm not going to end up like that right? No, you're not gonna end up like that. That was a movie it was, you know, embellished for Hollywood and, and even in its day, it was inaccurate, but even the more modern version of ECT, which involves succinylcholine, and other anesthetics, so that you're asleep, and you're not moving, so your brain is convulsing, and we're identifying that on an EEG a brainwave monitor, but we're not physically moving.
Steve Martorano
So in the bad old days, it was a kind of a blunt instrument to achieve the desired result?
Dr. Jonathan Beatty
Right. It's a sledgehammer to fix the clock. You know, the old-fashioned clock as opposed to, you know, a finer instrument. So, so TMS, I would argue, is this newer, finer instrument. So in this case, you're wide awake, there's no anesthesia involved, and you're pinpointing specific areas in the brain that you can actually access non-invasively. So it's an electromagnetic field that you can locate, this magnetic coil, on the scalp, and it has enough power to penetrate through the scalp and skull and get the magnetic field into certain areas in the brain. And we can identify those areas. For example, the motor cortex, which is you know, is fairly well understood. Different parts of the motor cortex, as you move along, say, from medial to lateral, you can find where they activate different parts of the body. We can use the magnetic field to identify, in most cases, we use what's called a thumb twitch, so the adductor pollicis muscle in your thumb, we get that to twitch, and we dial down the dosage or the power of the magnet to get it to what is the lowest possible dose or power strength of the magnetic field that will elicit that thumb switch. That's unique to you. So for one person, it might be 40. For another person, it might be 60. And the numbers aren't important, but just the difference between them.
Steve Martorano
You get a baseline for people.
Dr. Jonathan Beatty
You get a baseline, and then you calculate a strength. And then you use another anatomical landmark in order to identify this area in the brain called the dorsal lateral prefrontal cortex, which is more or less right about here. That's like a gateway to the other networks in the brain. And so this idea of networks we were talking about before, like the brain is just sort of a blob, what does it when you look at it grossly, what is it? But when you look at it functionally, when you can do these tests, you can see we right now seem that there are connections between different parts of the brain. So there are various networks in the brain, one of them called the default mode network that I alluded to earlier, has a lot of connection with the anterior cingulate cortex, which is a part of the brain in the front. Now, again, these names are not important to remember, but what's important to understand is that the DLPFC is a very superficial structure. So we can get the magnetic fields to reach that without hitting the entire brain. So instead of that, you know sledgehammer approach, we can use a finer instrument non-invasively, to get the right part of the brain that that then accesses these other critical functions.
Steve Martorano
So you're in a position now with a technique like TMS, to be able to, as you said, Get that baseline. So as an individual treatment for an individual person, locate, you already know the area of the brain that impacts whatever behaviors going on, and then raise or lower the magnetic force in that specific area. For something like depression, and addiction, you can do the same techniques?
Dr. Jonathan Beatty
Well, same techniques, slightly different protocol in terms of the pulse wave of the magnetic field changes somewhat, you know...
Steve Martorano
It's the same, it's the same idea.
Dr. Jonathan Beatty
Same idea, though, absolutely. And part of that has to do if you think about a repetitive loop in your head of, you know, let's say depression, where I'm really down in the dumps, my life is terrible, I can't get out of bed, I can't do anything, I everything I do fails, I'm no good. That's a really repetitive loop that a depressed person has that is essentially their default mode network. And their default mode network is highly connected to that other part of the brain that I mentioned, the anterior cingulate cortex, that part of your brain has to do with the future anticipation of pleasure. So if you think about, you know, tomorrow night, you're going out to dinner with your wife, and you're looking forward to it. On some level, that's a healthy ACC anterior cingulate cortex telling, you know, functioning properly, like this is something to look forward to tomorrow. If you're really depressed, you can't get to that because you're just stuck in this loop. And the TMS protocols can help kind of separate those two things so that the anterior cingulate can work properly without this repetitive loop. Interestingly enough, and we're gonna go into a different topic if we address this but psychedelics like psilocybin seem to do something similar to that they seem to kind of take that default mode network offline for a little while, not in, it's not permanent, but for even a few hours, enough that you then gain this new perspective like, "Hey, that's not me, that's just this weird loop." And then you can kind of access it differently along with talk therapy in those sessions, people are showing some interesting, you know, that's sort of another direction of the future of neuropsychiatry.
Steve Martorano
Yeah, we're hearing a lot about that. Now, our guest is Dr. Jonathan Beatty, he is a psychiatrist, he is treating people for a number of problems, from pain management to mood disorders to addiction, and he has joined us to really give us you know, what is the kind of the future of this, of this field of medicine, we are a long way, from the time when, if I were depressed, or having some other sort of behavior or mood disorder problems, were a long way from the time where the process began with someone saying, so tell me about your relationship to your mother.
Dr. Jonathan Beatty
Right and, and, you know, I just to clarify, I mean, you know, one of my mentors in training is a psychoanalyst, so he's a physician. He's a psychiatrist -- does not prescribe any medication -- strictly does psychoanalysis. It's remarkable how there is a place for that. So I don't want to discount that. I just want to clarify, I'm not.
Steve Martorano
First of all, as you know, a psychiatric examination is only as good as the person -- and this is true of any, any physician -- only is competent is the guy in front of you, the girl in front of you. It takes a special individual, who's sharp, understands the field, and is very empathetic, to use just the talk therapy to get to the bottom of anything. What's exciting about this is let's face it, it's more scientific. What's more, yeah, this is what we know. Let's see what we can do about it. You mentioned medicine I wanted we talked about TMS, which, by the way, you told me earlier, is an outpatient procedure, you go in for your regular visit, how's that work?
Dr. Jonathan Beatty
Exactly, right. So it's an outpatient procedure, you come into the office, you sit down in a chair, the equipment is there, it's again, non-invasive, you're wide awake the whole time, you could be if you wanted to read a newspaper, or listening to headphones of your favorite music. But again, you're alert and wide awake. And the technician whether it's me the as the physician in the room, or a technician, certain pieces of it need to be done by the medical provider. So that motor threshold and some of the more sort of technical logical aspects of it are done by the physician. And then the rest of it is often done by a technician in my office is done by a physician assistant. And so the procedure length is based on the protocol, there are protocols that are the shortest three minutes protocols that are as long as 37 minutes. The most common protocol I would say right now is a 19-minute protocol. And then yeah, as soon as it's finished. There's a coil that rests on your scalp. And it's if you've been in an MRI or ever seen when you hear that, like tap, tap, tap, tap, that is magnetic, the electromagnet inside the housing tapping against it, you know, against the inside wall, and you can hear that, although it's fairly quiet, you can definitely hear it and then you can feel it to a small degree, even though the housing is not moving because it's making contact and then the thing is tapping inside it. You can Dr. Jonathan Beatty a light tapping that's the sometimes people described as if...
Steve Martorano
You enter into an enclosure for this the way you would for an MRI?
Dr. Jonathan Beatty
Not at all. Nope, so you're sitting in a room in a chair, a comfortable chair that reclines and you know, it's sort of you know, it's a medical chair that where you can raise the legs and recline and so you're in a comfortable position with your arms on the armrests. And you're wide awake and you're looking around, you're not like enclosed in a claustrophobic type thing, the way that some people experience in MRI.
Steve Martorano
Here to talk about the use of medicines, which are referred to as MAT.
Dr. Jonathan Beatty
Yes.
Steve Martorano
Medical Assisted Treatment. They've been some great success in that. What can you tell us about how you use them in your practice?
Dr. Jonathan Beatty
Sure, well, even that, you know, we talked a little bit in this interview about the history of things and where the names for certain things come from and what they come to me now. So even MAT is sort of a funny term. So Medication-Assisted Treatment. Well, we don't treat heart disease with medication and refer to it as medication-assisted treatment, we refer to it as medical treatment. So it's this idea that MAT refers most commonly or most frequently with addiction. So it's the idea that we're taking something that was historically not medical. So we had a set of treatments that were nonmedical, and now we're going to try using medication to treat it. Which is sort of odd when you consider that it is a medical disease and that we are treating it as such. There are behavioral components to it which of course can be addressed in you know, more psychological type. There are certainly pharmacologic interventions, and so to speak to those in terms of addiction, one of the common ones that I use a lot is Naloxone. So that's an opioid antagonist, meaning that it blocks opioid receptors throughout your central nervous system -- certain subtypes of that opioid receptor more importantly. And it can be used and is FDA approved to treat both alcohol use disorder and opiate use disorder. The latter is a bit more obvious if you block opiate receptors. If you take an opiate, it's not going to work. You said alcohol use disorder. Yeah. What does that mean? You know, how does blocking an opiate receptor do anything to alcohol addiction? And the answer is, I don't entirely know and neither does anybody else. But to some extent, it seems like that the pleasure reward pathway is mediated through an endogenous opioid pathway in the brains of alcoholics. So when a non-alcoholic brain experiences intoxication, there is a degree of euphoria and enjoyment. It's not like overload. It's not high gear, it's enjoyable, but a lot of it is based on the surroundings, the social atmosphere, the experience of where you are the good meal, that it's complementing those things. In a nonalcoholic brain, they activate the pleasure reward pathway, but they're probably not doing much to the opioid pathway. An addicted brain, an alcoholic brain, it's more commonly through this opioid pathway, which if you block it, you diminish the euphoric effect of the alcohol and therefore reduce the association with that and therefore reduce that heavy drinking.
Steve Martorano
Isn't it also the case in addiction treatment that involves medicine or a technique that we don't know about yet? Also, benefits from talk therapy?
Dr. Jonathan Beatty
Absolutely. And so I should have even started off by saying that none of these medications is intended to be a silver bullet by itself. They're intended to be part of a comprehensive treatment program that includes psychosocial support. And there are other medications like for opioids, there's buprenorphine, you've certainly heard of methadone and methadone clinics that buprenorphine is an option that can be done in the office setting, whereas a methadone clinic is a special government-designated facility, anti-abuse, or disulfiram. That's for alcohol. So that's a very old drug that has a place but again, looks at it from a different perspective that was developed when that was just they all they understood was if we block an enzyme that breaks down alcohol, we leave it in a toxic state that makes you sick, if so, in other words, if you drink alcohol, you get sick. That's a punishment though, that's like you're a bad person, I'm going to give you this drug that makes you sick if you drink. So it's a punitive model. And if you didn't also complement that with talk therapy to explain No, we're not trying to punish you for that we're just trying to get the alcohol out of the way so that we can find out what else is going on. There are newer drugs like naltrexone, you know, which can work better. There's another one called Campral that has a place for alcohol, you know, and so this OBOT - it stands for Office-Based Opioid Treatment is a newer thing. I mean, newer, you know, a couple of decades at this point. But buprenorphine has been available and is now available in the long-acting injectable, there used to be an implantable form of it. And so these things can really help get the drug out of the way, or the substance out of the way. But then the work has to happen...
Steve Martorano
You want to make that we make that point a lot. You know, if you're in the grip of some addiction, and you find yourself in front of someone that says, this drug or this injection is all you need, then you're in front of the wrong person.
Dr. Jonathan Beatty
If somebody without addiction without any mental health issues, goes to the doctor and says oh, I, you know, I broke my ankle, okay, here's Percocet, and you get a month or two of Percocet or three and I see this, a lot of patients that come to me, this is how it started. It wasn't like they went out on the street looking for heroin. These were people that were highly functional, basically, you know, upstanding people in the sense that they weren't, they were going somewhere in their life, they weren't looking to fall into a drug addiction. Not that most people who become addicted are but some certainly do. But in this example, they get the Percocet and they get to take it and they like the way they feel from and they may or may not realize that But either way, they will eventually become physiologically dependent on it. And so if they didn't stop it abruptly, they're gonna have withdrawal and not know what it is. And so they might become addicted. And they might be somebody that you could just taper or use the buprenorphine to taper them off of it. And they may not need a lot of psychiatric or psychological intervention in terms of talk therapy, which would still probably be relevant, at least in the initial stages.
Steve Martorano
Sure.
Dr. Jonathan Beatty
There's not something that we're missing.
Steve Martorano
Dr. Beatty can we sort of wrap up here talking about the leading edge of what's going on with something you mentioned earlier, but I want to just get a little more detail about it. You referred to it in some notes to me during the week, as psychedelic psychiatry.
Dr. Jonathan Beatty
Sure.
Steve Martorano
There's been a lot written about that. Tell us what's going on there.
Dr. Jonathan Beatty
Absolutely. So that's something we're hearing and seeing a lot in the news. You know, as you alluded to earlier, a lot of people get their information about mental health and treatments through the news and good, bad, or otherwise, I mean Time Magazine, I believe just recently had it on their cover. So this idea of psychedelic psychiatry, which, you know, began its research in the 50s and 60s, but unfortunately, it was not done in a very proper manner, scientifically speaking, and ethically speaking. And that led to basically shutting down all of this research for decades. And then more recently, they've been doing some research and it's sort of coming back into focus. And they're identifying some really remarkable benefits to the application of certain psychedelic drugs such as psilocybin and what's in magic mushrooms, and LSD. Which is being researched, I think, in Israel for alcohol addiction. And now most recently in the United States, the MDMA, which is the active drug, that's an ecstasy, the club drug, and, and of course, ketamine, which is a dissociative anesthetic. So ketamine from I think was invented or approved in 1972 used during surgery, a very safe drug, in fact, used in children for surgery for decades. They've identified that this is actually something that can be helpful to treat depression. And now there is another form of it that's available to treat depression, I also use that in my office called SPRAVATO, or S ketamine. It's a nasal spray that the patient inhales
Steve Martorano
Wow.
Dr. Jonathan Beatty
And then they're under this sort of semi-anesthetic or subanesthetic state where they're a little bit sort of dreamy, for about 60 to 90 minutes. So they're in the office for two hours, actually. So they're monitored until they're completely resolved. And you know, interestingly enough, that's the sort of paradigm is just to have them sit there and you observe them. And that makes you know, you're just monitoring them. It's the sort of medical model. And this is, I guess, kind of tying into your question, what about incorporating, you know, sort of talk therapy. So it's not one or the other, but both that seem to show the best results. So what if we have either a psychiatrist or a psychotherapist that's able to talk with that person, while they're in this state where they're at default mode network is a little bit offline, they can access certain parts of the brain. And the patient who's suffering can actually have insight about those pieces of their brain or their experience that may be causing sadness or causing Post Traumatic Stress Disorder. So in the example of MDMA, it's Post Traumatic Stress Disorder. In phase three trials, 60% or more of these people who have 20-year histories of PTSD are no longer meeting the criteria.
Steve Martorano
Wow.
Dr. Jonathan Beatty
Now, mind you, that's 12 weeks of intensive psychotherapy, and in that about three sessions with MDMA. So like people are on MDMA all the time, this is three focalized sessions, they're about eight hours apiece with two therapists in the room...
Steve Martorano
Well, none of this is like methadone, which is a maintenance drug. These drugs, if they have any utility, will hopefully solve the problem with no further need for the drugs. It's a very exciting time, you know, we could do a whole other show. I mean, when you mentioned the irresponsibility, that the beginning of the psychedelic experiments if you're old enough, you know them. A couple of things happened after the creation in a laboratory of LSD that was not good. One was that the United -- you know, the Central Intelligence Agency immediately thought well, we can control people's minds. And of course, Timothy Leary, and a couple of other people said, "Oh, this is great. We'll just you know, have a great time and disrupt everything." And 15 minutes after that happened. the government said that's the end of it it's class one substance and you can't fool with it. So we're coming out from under that and hopefully doc and I know you'll agree with me on here we will get to a point it doesn't look like we are where these things go from being demonized to the pendulum swinging the other direction where suddenly there the appeal and end door of every problem we have. Marijuana is undergoing just that right now. Where it went from causing everything from you know, your hand...hair on your hands to pillaging and plunder to today we're being told we can cure everything. And that's certainly not the case either. Can we have you back many more times I have so many more questions about what you do and neuroscience and...
Dr. Jonathan Beatty
It was my honor and pleasure. I really enjoyed this and thank you so much for having me and I look forward to doing it again.
Steve Martorano
Appreciate it a lot Dr. Jonathan Beatty of you may become our in-house go-to guy when we talk about what's going on inside our heads. Thanks, Doc.
Dr. Jonathan Beatty
You got it.
Steve Martorano
Thanks as well. And don't forget to look for us everywhere you get your better podcasts. We appreciate it. See you next time on the Corner.
Retreat Behavioral Health
At Retreat Behavioral Health, we believe in the power of connection and quality care. We offer comprehensive holistic and compassionate treatment from industry-leading experts. Call 855-802-6600 and begin your journey today.
The Behavioral Corner
That's it for now. And make us a habit of hanging out at the Behavioral Corner and when we're not hanging follow us on Facebook, Instagram, and Twitter on the Behavioral Corner.
Subscribe. Listen. Share. Follow.
Recent Episodes